
Getting to the heel of the problem: plantar fascia lesions
T. Jeswania, J. Morleseb, E.G. McNallyc – Clinical Radiology (2009) 64, 931-939
Heel pain is a frequent disabling symptom. Clinical diagnosis is often difficult with a large range of possible diagnoses. Lesions of the plantar fascia form an important group. We present a review describing the common lesions of the plantar fascia, including plantar fasciitis, plantar fascia rupture, plantar fibromatosis, and plantar xanthoma, and illustrate them with appropriate magnetic resonance imaging (MRI) and ultrasound imaging. We also address foreign-body reactions, enthesopathy, and diabetic fascial disease.
Introduction Plantar fascia
The plantar fascia is a thick, multi layered, inelastic band of fibrous tissue that courses along the plantar surface of the foot. It contains medial, central, and lateral components. The term “plantar fascia” often refers to the large central component. This attaches to the medial tuberosity of the Os calcis and extends anteriorly becoming broader and thinner. In the region of the metatarsal heads, the plantar fascia divides into five processes, one for each of the toes. Each of these processes divides opposite the metatarsophalangeal articulation into two strata, superficial and deep. The superficial stratum of each process is connected to the dermis by skin ligaments (retinacula cutis). These ligaments reach the skin of the ball of the foot proximal to, and in the floors of the furrows that separate the toes from the sole. The deeper stratum divides into two slips that embrace the side of the flexor tendons of the toes. The lateral and medial portions of the plantar aponeurosis are thinner than the central portion, and cover the sides of the sole of the foot. Some authors refer only to two branches omitting the medial, but referring to the central as the medial. In this article, the three-branch approach will be used.
The primary function of the plantar fascia is to act as a bowstring and maintain the longitudinal arch of the foot.
Normal imaging anatomy
The normal plantar fascia is easily visualized using magnetic resonance imaging (MRI) or ultrasound. On plain radiography, the fascia can be seen between layers of surrounding fat, but its internal structure is not defined. Bony spur formation at the fascial origin is also seen on plain radiographs, but the presence of a spur does not necessarily indicate fascial disease. The normal plantar fascia is seen on MRI as a thin band with low signal intensity on all pulse sequences (Fig. 1). It is approximately 2–4 mm in thickness. Sagittal imaging allows optimal evaluation of the plantar fascia along its length. Coronal imaging is useful for assessing the size, shape, and internal signal characteristics of the fascia.

(a) The normal plantar fascia (red arrows) is seen as a thin band with low signal intensity on this STIR sequence and all other pulse sequences. (b) Sagittal, T1-weighted image showing a normal plantar fascia measuring 3 mm in diameter. (c) Coronal, PD, FS image showing the normal plantar fascia. The larger central cord (red arrow) is seen to measure less than 4 mm.
The plantar fascia is the most superficial of three connective tissue bands on the plantar aspect of the foot, the other two being the long and the short plantar ligaments. Flexor digitorum brevis muscle separates the plantar fascia from the long plantar ligament.
Lesions of the plantar fascia
The principle plantar fascia lesions are: plantar fasciitis, plantar fascia rupture, plantar fibromatosis, and plantar xanthoma. We will also address foreign-body reactions, enthesopathy, and diabetic fascial disease.
Plantar fasciitis/enthesopathy
Plantar fasciitis is the most common type of plantar fascia injury. It presents as pain on the underside of the heel. Patients often describe a sharp pain, generally worse after rest, especially on waking, worsening with the first steps, but lessening with progressive exercise. The two commonest causes are a misuse injury to the enthesis and inflammatory enthesopathy. Misuse injury refers to both overuse injuries seen in sport and normal use injury under excessive physiological conditions. The latter is most commonly seen in overweight, middle-aged patients. Inflammatory enthesopathy is associated with seronegative arthropathies, such as ankylosing spondylitis, Reiter’s disease, and psoriasis. Abnormalities in the fascia initially predominate at the plantar fascia origin. With chronicity the entire plantar fascia may become involved with thickening and nodularity. Acute traumatic injuries tend to predominate just distal to the insertion; however, given the similar aetiology, acute versus subacute repetitive trauma, it is unsurprising that there is some overlap in the imaging appearances.
Misuse injuries of the plantar fascia have been related to biomechanical derangement of the gait cycle, particularly during heel strike. The gait cycle can be divided into two phases, the stance and the swing. The stance phase is the interval in which the foot is on the ground. This can be divided into four further phases including: heel strike to flat foot; foot flat through midstance; midstance through heel off; and heel off to toe off. Problems with plantar fasciitis appear to stem from the heel strike phase. As the heel is placed on the ground whilst walking, the tibia rotates inwards and the foot is seen to pronate. This stretches the plantar fascia and flattens the arch of the foot. Repetition is thought to cause micro-tears in the plantar fascia with the central bundle most commonly affected. A similar aetiology is suspected in runners and jumpers.
An enthesis is the point of union between a tendon, ligament or capsule and bone. There are two different types of enthesis, fibrous and fibrocartilaginous. Fibrous entheses are characterized by pure, dense, fibrous connective tissue that links the tendon/ligament to the bone, but fibrocartilaginous entheses have a transitional zone of fibrocartilage at the bony interface. Most entheses are fibrocartilaginous, for example, those of the plantar fascia, annulus fibrosus, Achilles tendon, and most insertions on long bone epiphyses or apophyses. Typically, four zones of tissue are present: dense, fibrous connective tissue; uncalcified fibrocartilage; calcified fibrocartilage; and bone. The two fibrocartilage zones are separated by a calcification front known as the tidemark.
The MRI imaging characteristics of plantar fasciitis include: (1) fusiform thickening of the plantar fascia most commonly at its origin.1 and 2 (2) Increased signal within the fascia on both T1 and T2 sequences. The signal is often intermediate on T1 and proton density images with high signal on T2 or STIR images. (3) Oedema in the adjacent soft tissues. (4) Bony oedema within the Os calcis3 (Fig. 3), which is thought to be correlated with active disease and pain. There is some evidence that therapeutic intervention is more likely to be successful when bone oedema is present.4 (5) Bone spur formation.
Sagittal STIR sequences showing features of plantar fasciitis. The red arrow shows high signal within the proximal thickened plantar fascia with adjacent soft tissue and bony oedema.
The MRI features of enthesopathy show soft-tissue oedema at the enthesis with adjacent bony oedema (Fig. 5). The bony oedema is often associated with pain and is felt to reflect active inflammation at the enthesis. The typical early appearances of enthesopathy can be seen on ultrasound either within the ligament or adjacent bone. Within the ligament, the features are loss of the organized tendon structure and thickening. The ligament becomes hypoechoic and shows evidence of vascular in-growth, although this is uncommon in the case of the plantar fascia (Fig. 6). Changes are also seen in the adjacent bone with a combination of erosion and new bone formation. Erosion tends to occur at the sites of compression, such as the deep aspect of the plantar fascia. The earliest changes show irregularity of the bone surface where there is fine periosteal new bone formation.
The treatment of plantar fasciitis remains controversial. Conservative treatments include rest, non-steroidal anti-inflammatory agents (NSAID), physiotherapy, and orthoses. Steroid treatment has been shown to be effective in the short term as a treatment for plantar fasciitis.6 and 7 A Cochrane review showed an improvement in symptoms at 1 month but not at 6 months compared to a control group.8 Steroids have been described as altering the ultrasound appearances of plantar fasciitis by reducing plantar fascia thickness and decreasing the incidence of hypoechoic tissue, in addition to improving clinical parameters.9 Ultrasound guidance may be used to inject steroid and local anaesthetic for cases of plantar fasciitis. In the authors’ practice, the injection is given via a medial approach and placed on the deep aspect of the fascia, where it is more likely to be contained within the deep compartment and reduce the risk of fat necrosis. Ultrasound can also be used to guide dry-needle therapy, which may be a useful adjunct to corticosteroid injection that cannot be reliably carried out without image guidance. Recent papers have suggested the presence or absence of perifascial oedema may be helpful in guiding therapy10 with steroid injection showing better results in the presence of oedema and extracorporeal shock wave therapy (ESWT) better in its absence.
Other studies have shown subjective benefit from ESWT.11 Some have shown it to be relatively effective and a safe alternative treatment with improvements in pain and function scores.12
Randomized, prospective trials have shown benefit from foot orthoses and anterior night splints,14 with better compliance and less side effects reported with orthoses. Smaller trials have also suggested that oral NSAID therapy has a role in treatment when used within a conservative regimen.15
The use of autologous blood has been suggested as a method of inducing healing via cellular and humoral mediators.16 Recent trials have shown intra-lesional treatment can reduce pain and associated tenderness, but concluded steroid treatment remained superior in terms of speed and extent of improvement.
Surgery, such as plantar fascia release, is usually reserved as a last resort in the treatment of plantar fasciitis. Retrospective studies have shown an improvement in symptoms from surgery although they report up to 30% of patients having significant residual pain, restriction of activity and/or impaired function.17, 18 and 19
Plantar fascia rupture
The plantar fascia may rupture due to continued overuse when plantar fasciitis is present, or in relation to sporting injury in running/jumping athletes. Acute pain is usually experienced, which is often accompanied by a snapping/clicking noise.20 There is usually marked associated swelling. The majority of tears occur in the proximal fascia in the region of the Os calcis. The association between diabetes and an increased prevalence of plantar fasciitis and rupture has been suggested, although there is little research to support this. Up to 30% of patients give a history of previous steroid injections.21
The MRI imaging characteristics of plantar fascia rupture include: (1) complete or partial interruption of the low signal intensity plantar fascia with high T2/STIR signal. This is likely to represent haemorrhage, inflammation, and oedema (Fig. 7).20 (2) Occasionally there are associated injuries of the underlying flexor digitorum brevis muscle. This may manifest as high T1 and T2 signal representing haemorrhage and oedema.22
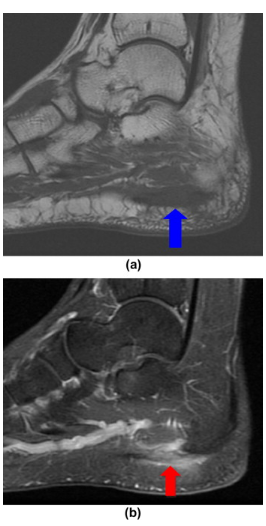
(a) Sagittal T1 and (b) sagittal STIR images showing evidence of partial rupture of the plantar fascia. There is evidence of partial interruption of the low signal intensity plantar fascia (red arrow) with high STIR signal and intermediate T1 signal (blue arrow). There is further high STIR signal surrounding the rupture, which is likely to represent haemorrhage, inflammation, and oedema. (Courtesy of Dr D. Resnick, San Diego, USA.)
The ultrasound characteristics of plantar fascia rupture include: (1) Disruption of the plantar fascia. In the authors’ experience, ultrasound is superior to MRI in differentiating true fibre interruption and tearing from oedema. (2) Hypoechoic tissue in the region of rupture due to inflammation/haemorrhage.
The differential diagnosis of plantar fasciitis includes several important conditions outlined below. A similar pain can occur due to neural compression. The nerve usually implicated is the first branch of the lateral plantar nerve, which may become trapped between flexor digitorum brevis and abductor hallucis longus. This is sometimes referred to as Baxter’s neuropathy. A positive Tinel’s sign at the site of compression may assist with the diagnosis. Other uncommon differentials include fat atrophy and traumatic fat necrosis.
The differential diagnosis of plantar fasciitis includes several important conditions outlined below. A similar pain can occur due to neural compression. The nerve usually implicated is the first branch of the lateral plantar nerve, which may become trapped between flexor digitorum brevis and abductor hallucis longus. This is sometimes referred to as Baxter’s neuropathy. A positive Tinel’s sign at the site of compression may assist with the diagnosis. Other uncommon differentials include fat atrophy and traumatic fat necrosis.
Plantar fibromatosis
This condition also known as Ledderhose disease is characterized by fibrous proliferation of the plantar fascia and is more common in men. There is an association with palmar fibromatosis (Dupuytren’s contracture). Like plantar fasciitis, plantar fibromas occur more commonly on the central component of the fascia. On examination, painless fibrous nodules can be palpated. They are frequently multiple and bilateral, which can be helpful diagnostically. Bilateral lesions have been described in 10–40% of cases.23 and 24 The differential diagnosis includes subcutaneous fat necrosis, implantation and dermoid, and foreign-body reaction. Troublesome lesions can be removed, although recurrence is common.
The MRI imaging characteristics of plantar fibromatosis include: (1) single or multiple nodular thickenings of the plantar fascia. They are low or intermediate signal intensity on both T1 and T2-weighted images (Fig. 9). (2) Larger lesions can have heterogeneous signal with a cicatrized appearance centred on the fascial band.22 (3) Infiltration of the plantar muscles can also be seen. (4) Variable contrast enhancement patterns have been described, although marked enhancement has been reported in up to 50% of lesions.25
Ultrasound has an important role in detecting small lesions that may not be apparent clinically. The demonstration of multiple and particularly bilateral lesions when only one lesion has been detected clinically is very important in limiting the differential diagnosis as there are few, if any, other conditions that present this pattern.
Other similar conditions include juvenile infantile fibromatosis and desmoid tumours. Juvenile infantile fibromatosis is a rare condition, which mainly affects children and adolescents. Fibrous tissue containing chondral elements is seen in the deep palmar fascia of the hand and wrist. Infiltration of local structures and bony erosion can be seen. Desmoid tumour, also known as fibromatosis, is a benign, but aggressive, lesion seen most commonly around the shoulder, pelvis, and abdomen. Lesions on MRI are isointense to muscle on T1 images and of high signal on T2-weighted images. Desmoid tumours often compress and engulf adjacent structures.
Foreign-body reaction
The differential diagnosis of a plantar fibroma includes a foreign-body reaction. A history of traumatic puncture is not always reported. The presence of reflective foreign material on ultrasound can assist in the diagnosis of this condition and removal may be attempted under ultrasound guidance. For deeper or fibrosed foreign bodies, a mark may be placed to help guide surgical removal. Foreign bodies have a variable appearance on MRI. A low signal on T1 is most common. Surrounding granulation tissue tends to have a high signal on T2-weighted images.
Plantar xanthoma
Xanthomas are seen in many hyperlipidaemia states. They represent collections of histiocytes that contain lipid. Involvement of tendons is most typical when disease tends to be bilateral and symmetric. Involvement of the finger extensors and the Achilles tendon (Fig. 11) is most typical. They are occasionally seen in the plantar fascia where they are usually asymptomatic, but can occasionally cause pain. Plantar fascia xanthomas are uncommon, and if this diagnosis is being considered for a plantar fascial mass, xanthomatous involvement of the Achilles tendon (Fig. 11) would be an expected finding. Patients can also find them unsightly and surgical removal is often for cosmetic and symptomatic reasons. Like fibromas there is a tendency for xanthomas to recur.
Calcaneal spurs
Calcaneal spurs usually originate from the medial calcaneal tuberosity at the attachment of the flexor digitorum brevis and abductor hallucis muscles; however, their sites of origin can be variable.26 Spurs may occur as a result of excessive repetitive traction by these intrinsic muscles, causing chronic micro trauma, which in turn, leads to periostitis and ossification. An association between spurs and numerous conditions including obesity, diabetes, acromegaly, and diffuse idiopathic skeletal hyperostosis (DISH) has been reported. Spurs may become symptomatic in the setting of plantar heel pad atrophy. Although calcaneal spurs have been described in association with plantar fasciitis, most publications conclude that they rarely cause this condition.1 Although a higher proportion of spurs is noted in plantar fasciitis, their presence is not specific. Plantar fasciitis may exist in the absence of a spur and asymptomatic spurs are common.
Conclusion
Plantar fascia lesions are responsible for a fair proportion of disabling heel pain. We have presented a review illustrated with MRI and ultrasound imaging in an attempt to highlight the variety of possible plantar fascial lesions. Although both imaging methods excel at imaging the plantar fascia, ultrasound has the added ability of allowing guided treatment at the time of imaging.
References
1
J.F. Berkowitz, R. Kier, S. Rudicel
Plantar fasciitis: MR imaging
Radiology, 179 (1991), pp. 665–667
Full Text via CrossRef | View Record in Scopus | Citing articles (110)
2
R. Kier
Magnetic resonance imaging of plantar fasciitis and other causes of heel pain
Magn Reson Imaging Clin N Am, 2 (1994), pp. 97–107
View Record in Scopus | Citing articles (42)
3
M. Steinborn, A. Heuck, M. Maier, et al.
MRI of plantar fasciitis
Rofo, 170 (1999), pp. 41–46
View Record in Scopus | Citing articles (10)
4
M. Maier, M. Steinborn, C. Schmitz, et al.
Extracorporeal shock wave application for chronic plantar fasciitis associated with heel spurs: prediction of outcome by magnetic resonance imaging
J Rheumatol, 27 (2000), pp. 2455–2462
View Record in Scopus | Citing articles (69)
5
E. Cardinal, R.K. Chhem, C.G. Beauregard, et al.
Plantar fasciitis: sonographic evaluation
Radiology, 201 (1996), pp. 257–259
Full Text via CrossRef | View Record in Scopus | Citing articles (117)
6
F. Crawford, D. Atkins, P. Young, et al.
Steroid injection for heel pain: evidence for short term effectiveness. A randomized controlled trial
Rheumatology, 38 (1999), pp. 974–977
Full Text via CrossRef | View Record in Scopus | Citing articles (91)
7
D. Atkins, F. Crawford, J. Edwards, et al.
A systematic review of treatments for the painful heel
Rheumatology, 38 (1999), pp. 968–973
Full Text via CrossRef | View Record in Scopus | Citing articles (56)
8
F. Crawford, C. Thomson
Interventions for treating plantar heel pain
Cochrane database Syst Rev, 3 (2003), p. CD000416
View Record in Scopus | Citing articles (32)
9
H. Genc, M. Saracoglu, B. Nacir, et al.
Long-term ultrasonic follow-up of plantar fasciitis patients treated with steroid injection
Joint Bone Spine, 72 (2005), pp. 61–65
Article | Purchase PDF | View Record in Scopus | Citing articles (46)
10
F. Sorrentino, A. Iovane, A. Vetro, et al.
Role of high resolution ultrasound in guiding treatment of idiopathic plantar fasciitis with minimally invasive techniques
Radiol Med (Torino), 113 (2008), pp. 486–495
Full Text via CrossRef | View Record in Scopus | Citing articles (11)
11
H. Gollwitzer, P. Diehl, A. Vonkorff, et al.
Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized controlled trial assessing the efficacy of a new electromagnetic shock wave device
J Foot Ankle Surg, 48 (2007), pp. 348–357
Article | Purchase PDF | View Record in Scopus | Citing articles (52)
12
C.J. Wang, F.S. Wang, K.D. yang, et al.
Long-term results of extracorporeal shock wave therapy treatment for plantar fasciitis
Am J Sports Med, 34 (2006), pp. 592–596
Full Text via CrossRef | View Record in Scopus | Citing articles (31)
13
M. Haake, M. Buch, C. Schoellner, et al.
Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial
BMJ, 327 (2003), p. 75
Full Text via CrossRef | View Record in Scopus | Citing articles (109)
14
E. Roos, M. Engstrom, B. Soderberg
Foot orthoses for the treatment of plantar fasciitis
Foot Ankle Int, 27 (2006), pp. 606–611
View Record in Scopus | Citing articles (49)
15
B.G. Donley, T. Moore, J. Sferra, et al.
The efficacy of oral nonsteroidal anti-inflammatory medication in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study
Foot Ankle Int, 28 (2007), pp. 20–23
Full Text via CrossRef | View Record in Scopus | Citing articles (44)
16
T.G. Lee, T.S. Ahmad
Intralesional autologous blood injection compared to corticosteroid injection for the treatment of chronic plantar fasciitis
Foot Ankle Int, 28 (2007), pp. 984–990
Full Text via CrossRef | View Record in Scopus | Citing articles (48)
17
M.S. Davies, G.A. Weiss, T.S. Saxby
Plantar fasciitis: how successful is surgical intervention?
Foot Ankle Int, 20 (1999), pp. 803–807
Full Text via CrossRef | View Record in Scopus | Citing articles (94)
18
W.D. Fishco, R.M. Goecker, R.I. Schwartz
The instep plantar fasciotomy for chronic plantar fasciitis. A retrospective review
J Am Podiatr Med Assoc, 90 (2000), pp. 66–69
Full Text via CrossRef | View Record in Scopus | Citing articles (12)
19
P.K. Vohra, R.J. Giorqini, E. Sobel, et al.
Long-term follow-up of heel spur surgery. A ten year retrospective study
J Am Podiatr Med Assoc., 89 (1999), pp. 81–88
Full Text via CrossRef | View Record in Scopus | Citing articles (21)
20
J.S. Yu
Pathologic and post-operative conditions of the plantar fascia: review of MR imaging appearances
Skeletal Radiol, 29 (2000), p. 491
Full Text via CrossRef | View Record in Scopus | Citing articles (14)
21
J.I. Acevedo, J.L. Beskin
Complications of plantar fascia rupture associated with corticosteroid injection
Foot Ankle Int, 19 (1998), p. 91
Full Text via CrossRef | View Record in Scopus | Citing articles (181)
22
J.A. Narvaez, J. Narvaez, R. Ortega, et al.
Painful heel: MR imaging findings
RadioGraphics, 20 (2000), p. 333
Full Text via CrossRef | View Record in Scopus | Citing articles (70)
23
M.J. Kransdorf, M.D. Murphey
Soft tissue tumors in a large referral population
M.J. Kransdorf, M.D. Murphey (Eds.), Imaging of soft tissue tumors (2nd ed.), Philadelphia: Lippincott Williams & Wilkins (2006)
24
T.H. Lee, K.L. Wapner, P.J. Hecht
Current concepts review: plantar fibromatosis
J Bone Joint Surg Br, 75 (1993), pp. 1080–1084
View Record in Scopus | Citing articles (56)
25
W.B. Morrison, M.E. Schweitzer, K.L. Wapner, et al.
Plantar fibromatosis: a benign aggressive neoplasm with a characteristic appearance on MR images
Radiology, 193 (1994), p. 841
Full Text via CrossRef | View Record in Scopus | Citing articles (67)
26
M.R. Abreu, C.B. Chung, L. Mendes, et al.
Plantar calcaneal enthesophytes: new observation regarding sites of origin, based on radiographic, MR imaging, anatomic, and paleopathologic analysis
Skeletal Radiol, 32 (2003), p. 13
Full Text via CrossRef | View Record in Scopus | Citing articles (21)


